Demography of paediatric renal care in Europe: organization and delivery
Jochen H. H. Ehrich1, Anita Amina El Gendi1, Alfred Drukker2, Jan Janda3, Constantinos Stefanidis4, Kate Verrier-Jones5, Jacqueline Collier6 and Manuel Katz7 1University Children’s Hospital, Medical School, Hannover, Germany, 2Division of Paediatric Nephrology, Shaare Zedek Medical Center, c/o POB 8504, Jerusalem, Israel, 3First Department of Paediatrics, Second Medical School, Charles University, Motol, Prague, Czech Republic, 4A & P Kyriakou Children’s Hospital, Athens, Greece, 5KRUF Children’s Kidney Centre for Wales, Cardiff, Wales, UK, 6Division of Child Health, Faculty of Medicine, University of Nottingham, UK and 7Maccabi Health Care Services, Primary Paediatric Care Unit, Soroka Medical Center, Ben Gurion University, Beer-Sheva, Israel
Abstract
Background: Members of the European Society of Paediatric Nephrology (ESPN) initiated a study of the demography and policy of paediatric renal care among European countries at the end of the 20th century.
Methods: A questionnaire was mailed to the presidents of each of 43 national renal paediatric societies or working groups in Europe. Data on each country’s population, income as reflected by its gross national product and infant mortality rate, were obtained from the United Nations. The paediatric health care systems were previously divided into three types: general practitioner care system, paediatric care system and combined care system (CCS).
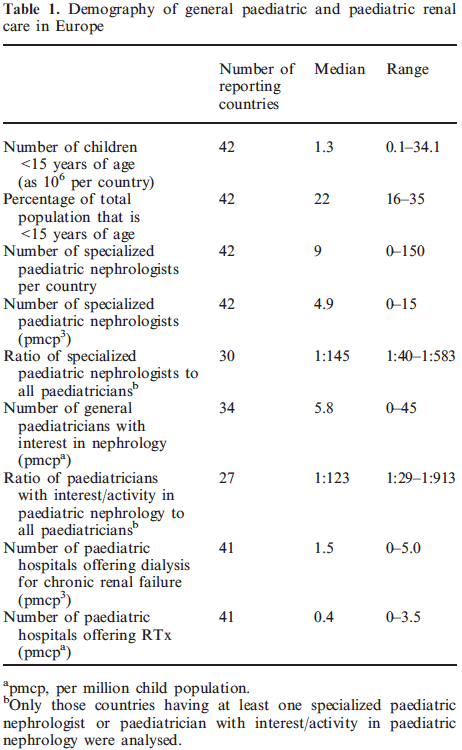
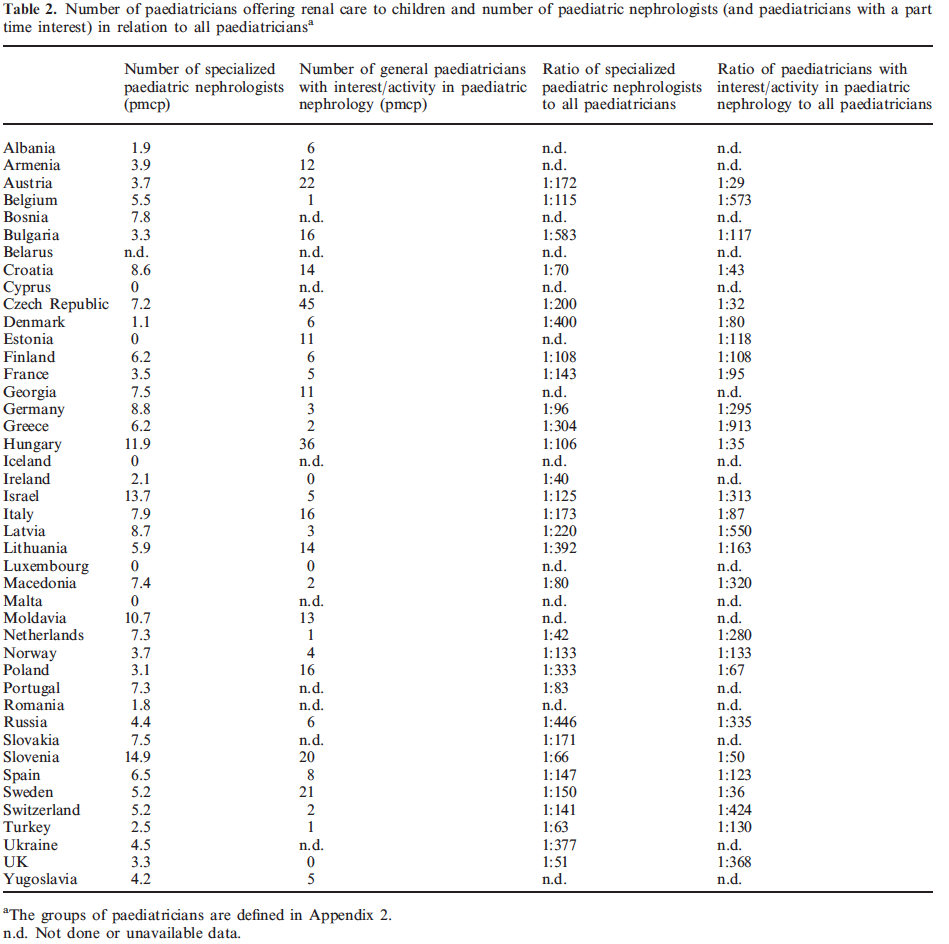
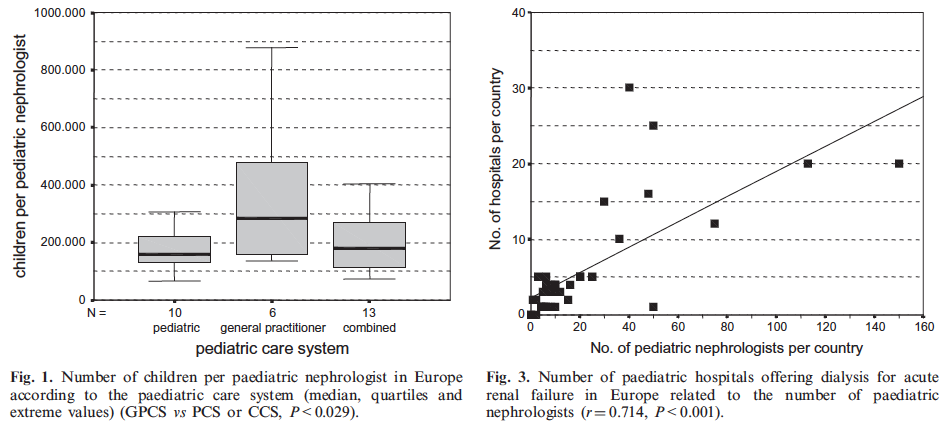
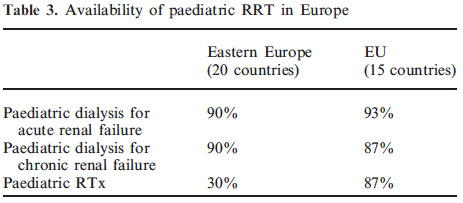
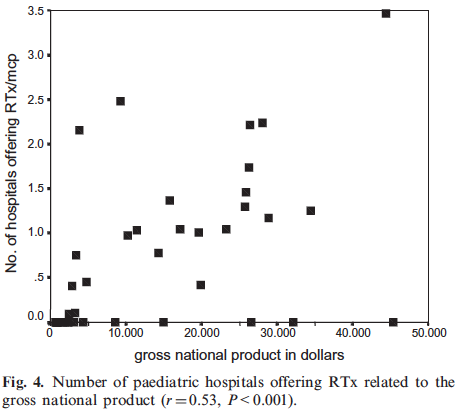
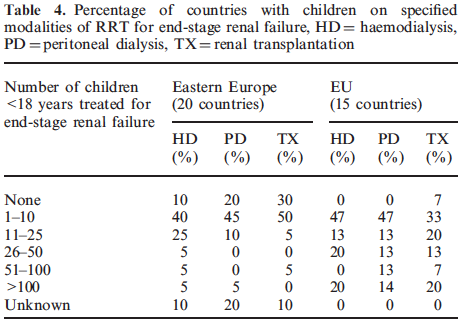
Results: In 1998, 842 specialized paediatric nephrologists worked in hospitals in 42 European countries. The median number of paediatric nephrologists per million child population (pmcp) was 4.9 (range 0–15). The median number of children served per paediatric nephrologist was significantly higher in countries with the general practitioner care system than in those with the paediatric or combined care system (CCS), namely 370 747 vs 169 456 and 191 788, respectively. In addition to specially trained paediatric nephrologists, there were 1087 paediatricians with a part-time interest/activity in paediatric nephrology in hospitals in 34 European countries. Eastern European countries had significantly more general paediatricians with part-time nephrological activities than countries belonging to the European Union (EU), 16.7 vs 6.6 pmcp. In 1998, 92% of 42 European countries offered paediatric dialysis facilities for acute renal failure and 90% for chronic renal failure and 55% offered paediatric renal transplantation (RTx). Only 30% of Eastern European countries (central omitted) offered paediatric RTx vs 87% of EU countries. The availability of paediatric RTx was associated significantly with the countries’ gross national product (r1/40.53, P<0.001). The median number of paediatric hospitals offering dialysis for childhood chronic renal failure was 1.5 pmcp (range 0–5.0) and the median number of paediatric hospitals offering paediatric RTx was 0.4 pmcp (range 0–3.5). Fewer children were on dialysis or were transplanted in Eastern European countries than in the EU.
Conclusions: At the end of the 20th century, there was a marked variation in delivery of paediatric renal care within Europe. This was related to factors such as size of the population, geographical and political situation, the type of primary paediatric care system and economic situation. European countries were far from equal with regard to access of renal replacement therapy for children. Improvement of the economic situation is beyond the capabilities of paediatric nephrologists. However, in these days of world-wide globalization paediatricians in greater Europe should be able to achieve better cooperation and exchange of ideas and information which would be the first step towards equality of renal care for children.
Keywords: co-operation; demography; European; health policy; paediatric nephrology; paediatric renal care; training
Introduction
On behalf of the Union of National European Paediatric Societies and Associations (UNEPSA), the demography of paediatric primary care in Europe was studied recently [1]. Three different patterns of paediatric primary care and community paediatrics in Europe were identified: the general practitioner care-system (GPCS), the paediatric care-system (PCS) and the combined care-system (CCS). In the present paper we address geographical and socioeconomic factors of paediatric renal care in European countries in 1998. This project was initiated by members of the European Society of Paediatric Nephrology (ESPN), which, as one of its goals, has set out to improve the availability and the standard of paediatric renal care in Europe. We hope to achieve this goal through the identification of and the response to the most urgent and relevant paediatric nephrology needs.
Methods
A letter explaining the purpose of the project, a list of definitions and a questionnaire were mailed in 1999 to a senior ESPN member of each of the 43 national paediatric nephrology organizations or working groups in Europe that are associated with the ESPN. The questionnaire contained 14 questions regarding delivery of care, treatment policies, cooperation and training of paediatric nephrologists (Appendix 1). Validation of the collected data was achieved by personal contacts with reporting colleagues and by discussions among past and present ESPN council members representing various European regions. A specialized paediatric nephrologist was defined as a paediatrician working full time in general paediatric nephrology, dialysis and paediatric renal transplantation (RTx) (Appendix 2). A paediatrician with a special interest/activity in nephrology was defined as a general paediatrician devoting part of his/her time to the care of children with common renal disease in settings without facilities for dialysis or RTx in children. In calculating the number of paediatric nephrologists, both part-time and fulltime employed paediatricians were included. Statistical data about population, country’s income and gross national product (GNP), as well as infant mortality rate (IMR) were obtained from UNICEF publications. Statistics included linear correlation, linear and multivariate regression. Student’s t-test, ANOVA, Mann–Whitney U, Kruskal– Wallis H and Pearson’s chi-square tests, for parametric and non-parametric data. The results were expressed as mean±SD and median plus range, respectively. A P-value <0.05 was considered significant.
Results
Unless otherwise stated the results are based on the responses from 42 out of 43 European countries (98% response rate); no data were available from Belarus.
Specialists
The total number of paediatric nephrologists in 42 European countries reported at the end of 1998 was 842, serving a child population <15 years of age of 169 million. In addition, there were 1087 general paediatricians with a part-time interest/activity in paediatric nephrology. Together with the specialized paediatric nephrologists, they provided basic renal care to approximately 150 million children <15 years of age in 34 out of 42 countries; no report was received from eight of these countries. The median number of specialized paediatric nephrologists was 4.9 pmcp (range 0–15) in 42 countries and the median number of general paediatricians offering renal care was 5.8 pmcp (range 0–45) in 34 countries (Table 1). Five of the 42 countries (Cyprus, Estonia, Iceland, Luxembourg, Malta) had no paediatric nephrologists, and renal care for children was supplied either by general paediatricians or by adult nephrologists (Table 2). Paediatric nephrologists were the only paediatricians seeing children with kidney disease in both the UK and Ireland. Excluding the five countries without specialized paediatric nephrologists, the number of children served by one specialized paediatric nephrologist ranged from 67 130 to 878 940 in the remaining 37 countries. Incorporating the above data into the previously described paediatric care systems [1] the number of children per specialized paediatric nephrologists showed significant differences (P<0.05) between countries with the GPCS and countries with the PCS or the CCS (Figures 1 and 2). Eastern European countries had significantly more general paediatricians with a parttime interest/activity for children with kidney diseases than European Union (EU) countries [16.6 vs 6.6 pmcp (P<0.05)]. The median ratio of specialized paediatric nephrologists to all practicing paediatricians in Europe was 1:145 (range 1:40–1:583) (Table 1). In countries with PCS the mean ratio of specialized paediatric nephrologists to practicing general paediatricians was significantly lower than in countries with the CCS and the GPCS (Figure 2 and Table 2).
Acute renal failure (ARF)
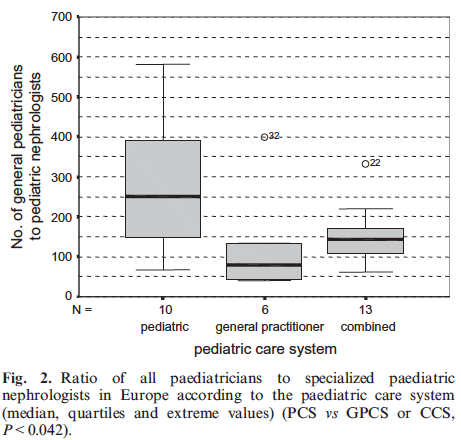
In 1998 there were 224 paediatric hospitals with dialysis facilities for ARF in 35 European countries. There were none in Albania, Cyprus, Estonia, Iceland, Luxembourg, Malta and Moldavia. Data on renal care for ARF—and chronic renal failure (CRF)—are set out below in different forms: expressed as hospitals/ country delivering that care, hospitals/pmcp of a given country, and hospitals related to <5 year mortality rate per country and according to GNP and IMR. The median number of paediatric hospitals offering dialysis for childhood ARF was 3.5 per country, range 0–30. The median number of paediatric hospitals offering dialysis for ARF was 1.7 pmcp (range 0–6.2). In 20 Eastern European countries the median number of hospitals offering dialysis for ARF in children was 1.7 vs 2.2 in 15 EU countries. These differences were not significant. The number of paediatric hospitals offering dialysis for ARF correlated positively to the size of the child population <15 years of age (r1/40.72, P<0.001) and to the number of paediatric nephrologists in the specific area/country (r1/40.71, P<0.001) (Figure 3); there was no association between the number of hospitals equipped to treat ARF in childhood and the three types of paediatric care systems. Countries with a mortality rate for children <5 years below 8.5 had a significantly (P<0.001) higher number of hospitals (2.4 vs 1.2 pmcp) offering dialysis for ARF in children than countries with a mortality rate above 8.5.
Chronic renal failure
A total of 179 paediatric hospitals offered dialysis for CRF in only 33 of the 41 countries. The countries with no dialysis for ARF also had no facilities for CRF; in Denmark dialysis for CRF in children was towards the end of 1998 only provided by adult units. The median number of paediatric hospitals offering dialysis for CRF was 1.5 pmcp (range 0–5.0). In Eastern European countries the median was 1.0 vs 1.6 in EU countries. The differences were statistically not significant. Countries with a GNP >8945 US$ showed a significantly (P<0.005) higher mean number of hospitals (1.9 pmcp) treating children with CRF than countries with a GNP <8945 US$ (1.1 pmcp) (Fig 4).
Renal transplantation
Fifty-five percent of the 42 European countries offered RTx for children <15 years of age in specialized paediatric hospitals, there being major differences between EU countries (12/15), Eastern European countries (6/20) and others (4/7) (Table 3). The median number of paediatric hospitals offering RTx was one per country, ranging from 0 to 20. We identified 99 paediatric hospitals offering RTx in Europe. The median number of paediatric hospitals offering RTx was 0.4pmcp (range 0–3.5). In countries with the PCS, 58% had paediatric hospitals with facilities for childhood RTx compared to 67% of countries with the CCS, and to 83% with the GPCS. Eighty-one percent of countries with a GNP >8945 US$ provided paediatric RTx and only 29% of countries with a GNP <8945 US$ (P0.001). Countries with a GNP >8945 US$ had a significantly (P<0.001) higher mean number of hospitals specializing in RTx (1.2 pmcp) than countries with a GNP <8945 US$ (0.2pmcp).
Insurance
Differences in access to renal replacement therapy (RRT) related to the different health insurance systems (public, mixed and private). The public insurance system had a lower number of doctors involved in end-stage renal disease (ESRD), and the highest proportion of transplanted vs dialysed children.
Registry
In 1996, 28 out of 40 European countries (70%) reported data on RRT in their young patients either to a national and/or multinational registry. Fewer Eastern European countries than EU countries reported data on renal patients to the various registries (50 vs 100%). High quality registry data fulfilling the criteria of completeness and accuracy were not available for the majority of countries reporting to the registries. Unfortunately, our own data on children receiving either haemodialysis, peritoneal dialysis or a RTx in 1996 (Table 4) can also only be taken as an estimate given by the national representatives answering the questionnaire. Nevertheless, our data show without any doubt that considerably fewer children were dialysed or transplanted in Eastern European countries than in the EU.
Needs
Seventy-one percent of all responding paediatric nephrologists stated that their country needed more paediatric nephrologists (1–10 nephrologists in 50% of countries and >10 in 21%), and 50% asked for more dialysis nurses (1–10 nurses in 25% of countries and 11–25 in 25%). The need for more personnel correlated neither with geographical and economic factors nor with the three paediatric care systems. Eighty-six percent of national representatives considered RRT essential for their patients with CRF. Representatives from Armenia, Georgia, Lithuania, Luxembourg and Moldavia stated that chronic RRT was not a national priority in paediatric care in 1998.
Congresses
Forty-eight percent of 42 countries reported having regular national paediatric nephrology congresses for their members, 33% had no regular meetings; no data were available for 19% of countries reporting.
Discussion
'Health care for all by the year 2000’ as prophesized by the World Health Organisation, was not achieved world-wide or in Europe. This holds true for the health of children, despite the fact that when the last century came to a close, 170 000 paediatricians were caring for a paediatric population of >150 million children <15 years of age, living in 42 European countries. General paediatric primary care in these countries was the subject of a previous publication in this journal [1].
To the best of our knowledge this is the first study undertaken to evaluate the demography of specialized paediatric renal care in these 42 European countries. In doing so, the paper answers the suggestions proposed in 1991 by our colleague Sir Cyril Chantler [2] who stated that the role of paediatric nephrologists in different European countries requires closer examination. He also proposed that Europe needs to agree upon appropriate and equal training in paediatric nephrology. In fact, ESPN recently published training recommendations, part of which is included in Appendix 2 [3]. Such a training programme has not yet been fully realized. Therefore, in 1998 and even at the time of writing (2003), the situation showed a great diversity in the ability and training of paediatric nephrologists in Europe, and even more among paediatricians with an interest in nephrological activities. When we, the authors, therefore write about these two categories of paediatric care-providers, we are well aware of the lack of homogeneity among these two groups. This is only one of the many problems we faced in accumulating the reported data which are long overdue. However, it must be realized that coordination between many countries and assuring the reporting of reliable data, has taken much more time than was anticipated. Our data, therefore, refer only to the state of renal paediatric care in 1998. We are presently in the process of updating these data. One of the major problems facing us when accumulating the above data, was the lack of demographic data on the incidence and prevalence of all renal diseases in childhood in Europe. We have reliable estimates, obtained from the European Dialysis and Transplant Association (EDTA) Registry in 1991, on the number of children starting RRT per year, which ranged between 5 and 14 children pmcp in different European countries [4]. When assuming a median number of eight children per year/pmcp we can predict, on the basis of these 12-yearold registry data, that 1000 children will probably have to start RRT every year in Europe.
There is a long-standing argument in the academic literature as to who should be the preferred doctor treating children with special, organ-centred, diseases. It has been argued by many paediatric nephrology societies that children should be treated by specialized paediatric nephrologists. Adult nephrologists have agreed with these demands as evidenced by the fact that in 1989 >90% of children <15 years of age with ESRD were treated in specialized paediatric nephrology centres in Europe [4–6]. In this regard we have to stress the differences found between the Eastern European and EU countries. The former had less paediatric nephrologists working in dialysis or transplantation and more paediatricians with part-time paediatric nephrology activities. The latter may be due to the fact that Eastern countries had more general paediatricians than Western countries [1]. Only 30% of Eastern countries offered RTx vs 87%of EU countries. In many Eastern European countries the care of children needing dialysis and RTx was not in the hands of paediatric nephrologists. Boesken et al. [7] and others [8] stated that there were three types of specialists practicing adult nephrology in countries of the former Soviet Bloc: a therapeutist (nephrologist), who treated general nephrology problems, a dialysis specialist who was often a surgeon, and a transplant surgeon. Renal biopsies were more often done by urologists than by nephrologists. This fragmentation of nephrology was also seen in Eastern European paediatric nephrology as reported by the presidents of national societies and working groups (personal communications). These differences lead to the conclusion that many paediatric nephrologists in Eastern Europe would not be considered paediatric nephrology specialists in EU countries. Considering the division of paediatric nephrology services in Eastern Europe, it is certainly reasonable to aim at an integration of services (the opposite of fragmentation) and this has recently effectively been achieved in the Czech Republic, Hungary and Poland [9–11]. In these countries this process took rather long because of: (1) the time needed to train the paediatric nephrologists, (2) realizing the necessary organizational steps which included convincing the authorities at government level of the reduced costs of integrated care, and (3) convincing national medical organizations to make changes in their training programmes.
It may well be that the 842 paediatric nephrologists together with 1087 paediatricians with renal interest, are enough to supply renal care to every child in Europe. However, many may still not be adequately trained. If training programmes are organized locally and are integrated by a central European body like the Union of the European Medical Subspecialists (UEMS), the overall situation should rapidly change for the better. This is one of the main recommendations of our paper. In addition to this recommendation, we strongly feel that the training programmes for paediatric nephrology should not in any way be related to any changes in the three paediatric care systems [1]. Differences in access to RRT are not only related to these defined three paediatric health care systems but also to GNP, and obviously the local health insurance systems of the various countries. Eighty percent of countries with the GPCS had public health insurance. Data from adult nephrology patients show that in comparison to the private and mixed systems, the public insurance system had a lower number of doctors involved in ESRD, lower take-on rates for RRT and a higher proportion of transplanted patients [12]. There is no reason to doubt that this also holds true for children with renal disease.
Health care expenses have grown steadily over the past 15 years, including those for RRT and specifically for RTx. It is thus not surprising that all current reform efforts centre on cost and cost control. Public health physicians and health policy makers evaluate many clinical interventions for their effectiveness. Few are as effective as RRT, without which patients with ESRD will die. Data on the cost of RRT in Europe are scant. Adult services were mainly evaluated and they do not link outcome measures with costs and resource use. Furthermore, they only analyse the direct cost of treatment modalities without assessing the whole spectrum of care in renal failure. RRT in children is known to be more expensive than in adults [13], due to many factors such as the higher numbers of doctors and nurses needed per treated child, more personnel for psychosocial care, teachers, growth hormone therapy and special diets for the very young. The total budgetary costs for all paediatric ESRD patients are, however, much less than for adults [14] for the simple reason that the incidence and prevalence of ESRD in children are much lower than in adults. The costs of various treatment modalities may vary from country to country and are undergoing rapid changes requiring continuous adaptation of position papers [15]. Vecchi et al. [16] attributed differences in modality selection such as haemodialysis or peritoneal dialysis to differences in micro-economics of the provider. Haemodialysis is a treatment with a high fixed cost (personnel and structure) whereas peritoneal dialysis is a treatment modality with low fixed costs but high variable costs (supplies) and less need for investment. This may be the reason why peritoneal dialysis was more expensive in Eastern than in Western European countries. To expand on this, it has to be realized that new pharmaceuticals, of which 90% are produced in 10 countries (Europe, Japan, USA), and all the necessary supplies for peritoneal dialysis including lines, bags, fluids, connectors, etc., have to be imported from Western countries. These variable costs constituted the majority of expenses for peritoneal dialysis in Eastern Europe whereas the fixed costs (e.g. salaries) were much less and therefore haemodialysis was often cheaper in Eastern Europe [6,17,18]. RTx remains the treatment of choice for children with ESRD, not only with regard to survival and quality of life, but also as far as long-term costs are concerned [13,19].
Europe, at the end of the 20th century was found to be unequal, as far as access of children and adolescentsto RRT is concerned, both for ARF and CRF. This was proven to be due to different national financial constraints and local priorities in health care. To what extent the goal of equal access to RRT throughout Europe has to be modified is an issue for discussion. Very few of our reporting colleagues stated that RRT was not a priority in their country, possibly reflecting a gap between wishful thinking and reality. In some Eastern European countries, the numbers of dialysis and transplant facilities for adults have increased significantly in the last decade. The paediatric share of this development is not yet clear. In 1995, it was estimated that only 3% of all children with ESRD received appropriate treatment in countries of the former Soviet bloc [6]. In 1998, there were indications that fewer children than adults had access to RRT. The fact that, according to our data, 90% of all European countries provided paediatric dialysis for CRF but only 55% offered paediatric RTx, is disturbing. We have no explanation for this paradox. When reviewing national reports on RTx from Eastern European countries, several reasons were given for the underdevelopment of their RTx programmes. Slovenia had a low procurement of cadaveric kidneys. Albania was faced with financial constraints and a lack of infrastructure, trained personnel, and public cooperation [20,21]. In Romania all kidneys for RTx came from living related donors [22] whereas Polish paediatric surgeons reported in 1996 that only 0.8% of all kidney transplants and 7.9% of paediatric RTx were performed from living related donors [23].
In this paper we have discussed some aspects of the organization and delivery of paediatric renal care in Europe and the challenges awaiting European paediatric nephrologists in the years to come. These challenges include: more individual initiative and cooperation, regular and repeated international training courses organized by the ESPN in Eastern European countries, the establishment and continuous funding of rescue teams for treatment of (epidemic) paediatric ARF wherever these are needed, formation of an ethical consensus committee, a well functioning European registry and/or national registries, an agency for paediatric nephrologists (facilitating job opportunities throughout Europe), and a task force on standardization of diagnosis and therapy of renal diseases in children. Paediatric nephrologists should realize that, depending on the local circumstances, they may well not be the only primary care-givers for children with renal disease. They should therefore aim for cooperation with all necessary medical personnel and institutions, to obtain the best care for their patients. At the same time, they should continue in their time-honoured role, that of setting the standards in paediatric renal care.
Conclusion
In Europe, the health care of children with kidney diseases varied greatly in 1998, between and within countries. Economic, geographical and historical factors contributed to the intrinsic and extrinsic variations, as well as the different systems of primary paediatric care. The number of specialized paediatric nephrology centres per country (defined as centres offering general paediatric nephrology, dialysis and RTx) is difficult to assess. It would seem that a median number of 1.5 centres pmcp with four paediatric nephrologists per centre providing 24 h service may suffice [4]. Paediatric nephrologists in greater Europe should try to achieve better cooperation and exchange of ideas and information to improve renal care in all children and to decrease unnecessary variations in management. Acknowledgements. We are indebted to the representatives of 42 European national paediatric nephrology societies, associations or working groups for providing us with the data reported in this paper: Balzar and Ring (Austria); Berg (Sweden); Biver and Soergel (Luxemburg); Bogdanovic (Yugoslavia); Brumario (Romania); Cemerlic-Zecevic (Bosnia); Drukker (Israel); Ehrich (Germany); Erling (Denmark); Famina (Ukraine); Gill (Ireland); Gruenberg and Traat (Estonia); Guignard and Bianchetti (Switzerland); Holmberg (Finland); Horkelsson (Iceland); Ignatova and Tsygin (Russia); Janda (Czech Republic); Kaltenis (Lithuania); Kenda (Slovenia); Kovacs (Slovakia); Lilova (Bulgaria); Loirat (France); Moghal and McGraw (UK); Monn (Norway); Monnens (the Netherlands); Ozen and Bakkaloglu (Turkey); Pagava and Rzchiladse (Georgia); Proesmans (Belgium); Puretic (Croatia); Reusz (Hungary); Rizzoni (Italy); Rosa (Portugal); Rusnac (Moldavia); Santos and Malaga (Spain); Sarkissian (Armenia); Sieniawska (Poland); Stefanidis (Cyprus, Malta); Stefanidis and Constantopoulos (Greece); Strazdins (Latvia); Tasic and Kuzmanovska (Macedonia); Xhepa (Albania). Conflict of interest statement. None declared.
References
1. Katz M, Rubino A, Collier J, Rosen J, Ehrich JHH. Demography of paediatric primary care in Europe: delivery of care and training. J Pediatr 2002; 109: 788–796
2. Chantler C. Paediatric nephrology on the threshold of European integration. Pediatr Nephrol 1991; 5: 428–432
3. European Society for Paediatric Nephrology. Recommendations for the training of European Paediatric Nephrologists by the European Society of Paediatric Nephrology. Pediatr Nephrol 2001; 6: 192–195
4. Loirat C, Ehrich JHH, Geerling W et al. Report on management of renal failure in children in Europe, XIII, 1992. Nephrol Dial Transplant 1994; [Suppl 1]: 26–40
5. Ehrich JHH, Rizzoni G, Brunner FP et al. Combined report on regular dialysis and transplantation of children in Europe 1989. Nephrol Dial Transplant 1991; 6 [Suppl]: 37–47
6. Mehls O, Rigden S, Ehrich JHH, Berthoux F, Jones EHP, Valderabano F. Report on management of renal failure in Europe, XXV, 1994. The child–adult interface. Nephrol Dial Transplant 1996; 11 [Suppl 1]: 22–36
7. Boesken WH, Ahmed KEY, Me´ry JP et al. Observations on renal replacement services in Russia, Belarus and Lithuania. Nephrol Dial Transplant 1995; 10: 2013–2016
8. Lazovskis I. Nephrology, dialysis and renal transplantation in Latvia: problems of our specialty in a country of the former Soviet Bloc. Nephrol Dial Transplant 1994; 9: 214–216
9. Rutkowski B on behalf of the Central and Eastern European Advisory Board in CRF and Scientific Advisory Board of the ERA-EDTA Registry. Changing pattern of end-stage renal disease in central and eastern Europe. Nephrol Dial Transplant 2000; 15: 156–160
10. Rutkowski B, Puka J, Lao M et al. Renal replacement therapy in an era of socioeconomic changes-report from the Polish registry. Nephrol Dial Transplant 1997; 12: 1105–1108
11. Editorial. The Czech Society of Nephrolopgy—an introduction. Kidney Blood Press Res 2000; 23: 73–74
12. Ho¨ rl WH, Alvaro F, Williams PF. Healthcare systems and end stage renal disease (ESRD) therapies, an international review: access to ESRD treatments. Nephrol Dial Transplant 1999; 14 [Suppl 6]: 10–14
13. Arnold W, Alexander S. Cost, reimbursement and the paediatric nephrologist in the United States Medicare/End-Stage Renal Disease Program. Pediatr Nephrol 1997; 11: 250–257
14. Neuhaus TJ, Goetschel P, Leumann E. Small patients—high costs: economic aspects of medical treatment of children with early onset of chronic renal failure. Praxis 1998; 87: 1593–1599
15. Chesney RW, Arrant BS Jr, Hirschmann G, Jose PA, Novello AC, Siegel AJ. Position paper on current status and future needs of paediatric nephrology in the United States: training and research. Pediatr Nephrol 1989; 3: 372–380
16. Vecchi AF, Dratwa M, Wiedemann ME. Healthcare systems and end-stage renal disease (ESRD) therapies-an international review: costs and reimbursement/funding of ESRD therapies. Nephrol Dial Transplant 1999; 14 [Suppl 6]: 31–41
17. Ursea N, Mircescu G, Constantinovici N et al. Nephrology and renal replacement therapy in Romania. Nephrol Dial Transplant 1997; 4: 684–690
18. Rizzoni G, Broyer M, Ehrich JHH et al. The use of continuous peritoneal dialysis in Europe for the treatment of children with end-stage renal failure: data from the EDTA Registry. Nephrol Dial Transplant 1990; 5: 985–990
19. Broyer M, Chantler C, Donckerwolcke R, Ehrich JHH, Rizzoni G, Scha¨ rer K. The paediatric registry of the European Dialysis and Transplant Association: 20 years experience. Pediatr Nephrol 1993; 7: 758–768
20. Kandus A, Buturovic-Ponikvar J, Febren A. Kidney transplantation in Slovenia from 1986 through 1991. Transplant Proc 1992; 26: 2430–2431
21. Myaftar B, Nestor T. Living donor transplantation: ethical, social, legal and religious aspects in Albania. Transplant Proc 1996; 28: 3582–3583
22. Ursea N, Mircescu G, Constantinovici N et al. Nephrology and renal replacement therapy in Romania. Nephrol Dial Transplant 1997; 4: 684–690
23. Kalicinski P, Grenda R, Smirska E, Kaminski A, Prokurat A. Living-related donor kidney transplantation in children: child’s health center memorial hospital experience. Transplant Proc 1996; 28: 3575 Received for publication: 19.1.04 Accepted in revised form: 7.4.04
Appendix 1. Questionnaire on paediatric renal care in 1998 in Europe
Part I. Demography questionnaire
- How many paediatric nephrologists in your country are working in a hospital?A paediatric nephrologist is defined as a doctor with 2–3 years of special training in nephrology (including dialysis and renal transplantation),after qualifying as a general paediatrician. Please give the most accurate number of paediatric nephrologists.
- How many paediatricians in your country are general paediatricians with a special interest and part-time work in paediatric nephrology?Please give the most accurate number of paediatricians.
- Do the paediatric nephrology units in your country report to a Registry on renal replacement therapy in children?Enter ‘1’ for yes, ‘2’ for no and ‘9’ for unknown. If yes, please specify which registries.
- How many specialized paediatric nephrology centres offering dialysis/and or paediatric kidney transplantation existed in your country in 1998? Please give their number.
- Do you have paediatric hospitals in your country offering dialysis (any type) to children with acute renal failure?
Enter ‘1’ for yes, ‘2’ for no. If yes, please give their number.
- Do you have paediatric hospitals in your country offering dialysis (any type) to children with chronic renal failure?
Enter ‘1’ for yes, ‘2’ for no. If yes, please give their number.
- If you offer dialysis for chronic renal failure, how many children <18 years with end-stage renal failure were treated with haemodialysis on 31st December, 1996 in your country? Enter ‘1’ for 1–10, ‘2’ for 11–25, ‘3’ for 26–50, ‘4’ for 51–100, ‘5’ for 101–250 and ‘6’ for >250 children. Enter ‘9’ for other or unknown (please specify). Estimation 1/4 1, registered data 1/4 2.
- How many children <18 years with end-stage renal failure were treated with CAPD/CCPD on 31st December, 1996 in your country? Enter ‘1’ for 1–10, ‘2’ for 11–25, ‘3’ for 26–50, ‘4’ for 51–100, ‘5’ for 101–250 and ‘6’ for >250 children. Enter ‘9’ for other or unknown (please specify). Estimation1/41, registered data1/42. 304 J. H. H. Ehrich et al.
- Do you have paediatric hospitals offering renal transplantation to children with chronic renal failure in your country? Enter ‘1’ for yes, ‘2’ for no. If yes, please give their number.
- How many children <18 years with end stage renal disease received a kidney transplant in 1996 in your country? Enter ‘1’ for 1–10, ‘2’ for 11–25, ‘3’ for 26–50, ‘4’ for 51–100,‘5’ for 101–250 and ‘6’ for >250 children. Enter ‘9’ for other or unknown (please specify). Estimation1/41, registered data1/42.
Part II. Policy questionnaire
- How many more paediatric nephrologists would be needed in the hospitals of your country to provide a complete service everywhere? Enter ‘0’ for none, ‘1’ for <10, ‘2’ for 11–25, ‘3’ for 26–50, ‘4’ for 51–100, ‘5’ for 101–250 and ‘6’ for >250 paediatric nephrologists. Enter ‘9’ for other or unknown (please specify).
- How many more dialysis nurses would be needed in the hospitals of your country? Enter ‘0’ for none, ‘1’ for <10, ‘2’ for 11–25, ‘3’ for 26–50, ‘4’ for 51–100, ‘5’ for 101–250 and ‘6’ for >250 dialysis nurses. Enter ‘9’ for other or unknown (please specify).
- Compared to the priorities of paediatric care in yourcountry, do you regard a renal replacement therapy programme for children with renal failure as essential?
A. for treating acute renal failure: ‘1’ for yes, ‘2’ for no,
B. for treating chronic renal failure: ‘1’ for yes, ‘2’ for no.
- Are there regular meetings of paediatric nephrologists in your country? Enter ‘1’ for yes, ‘2’ for no.
Appendix 2. Definitions
Paediatricians are defined as physicians who finished their formal training in paediatrics licensed by the local health authorities or academic bodies in the country (either after undergraduate or as postgraduate’s training). Paediatric nephrologists are defined as licensed paediatricians with a minimum of 3 years training including experience in neonatology and intensive care plus a higher 3 years specialty training in paediatric nephrology in out- and in-patient settings (which may also include adult nephrology). Part of the 3 years may be obtained during the period of general paediatric training. During the training the European Society for Paediatric Nephrology has suggested that a high standard of expertise should be obtained in: The embryology of the kidney and the urinary tract. The anatomy, histopathology and physiology of the kidney and its circulation under normal and abnormal conditions. The pathology and pathophysiology of congenital and acquired diseases of the kidney and the urinary tract in the growing child. The aetiology, symptomatology, diagnosis and differential diagnosis of congenital and acquired renal diseases in the fetus, infant, and child and their appropriate investigation by imaging, renal function tests and renal histopathology. The performance or detailed knowledge of the following procedures: renal biopsy, renal ultrasonography, renal clearance techniques, peritoneal dialysis and haemodialysis, continuous haemofiltration, dietary and drug adjustment for the treatment of paediatric renal disease and renal transplantation. During the training period the trainee should acquire knowledge of the indications and management of surgical interventions in the urinary tract and of renal transplantation. A good understanding of the causes of bladder voiding abnormalities, their cystometric investigation and their medical and surgical treatments. A good understanding of the prevention, manifestations and management of psychosocial problems which arise in children with chronic renal disease and their parents/caretakers. This should include awareness of ethical issues. Paediatricians with an interest in paediatric nephrology are defined as licensed general paediatricians with a special interest and part-time work in paediatric nephrology. Within the primary care system for children we previously defined three subgroups according to the proportion of children aged <15 years seen by either paediatricians or family physicians/general practitioners (GPs) [1]: The paediatric system has >75% of children under the care of paediatricians. The general practitioner/family doctor system has >75% children seen by family physicians/GPs. The combined system has both paediatricians and GPs offering primary care to almost equal numbers of children.
Click here to download the presentation



