Paediatric primary care in Europe: variation between countries
Diego van Esso,1 Stefano del Torso,2 Adamos Hadjipanayis,3 Armand Biver,4 Elke Jaeger-Roman,5 Bjorn Wettergren,6 Alf Nicholson7; and the members of the Primary– Secondary Working Group (PSWG) of the European Academy of Paediatrics (EAP)
Abstract
Background
Although it is known that differences in paediatric primary care (PPC) are found throughout Europe, little information exists as to where, how and who delivers this care. The aim of this study was to collect information on the current existing situation of PPC in Europe.
Methods
A survey, in the form of a questionnaire, was distributed to the primary or secondary care delegates of 31 European countries asking for information concerning their primary paediatric care system, demographic data, professionals involved in primary care and details of their training. All of them were active paediatricians with a broad knowledge on how PPC is organised in their countries.
Results
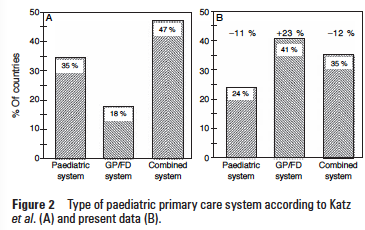
Responses were received from 29 countries. Twelve countries (41%) have a family doctor/ general practitioner (GP/FD) system, seven (24%) a paediatrician-based system and 10 (35%) a combined system. The total number of paediatricians in the 29 countries is 82 078 with 33 195 (40.4%) working in primary care. In only 15 countries (51.7%), paediatric age at the primary care level is defi ned as 0–18 years. Training in paediatrics is 5 years or more in 20 of the 29 countries. In nine countries, training is less than 5 years. The median training time of GPs/FDs in paediatrics is 4 months (IQR 3–6), with some countries having no formal paediatric training at all. The care of adolescents and involvement in school health programmes is undertaken by different health professionals (school doctors, GPs/FDs, nurses and paediatricians) depending on the country.
Conclusions
Systems and organisations of PPC in Europe are heterogeneous. The same is true for paediatric training, school healthcare involvement and adolescent care. More research is needed to study specific healthcare indicators in order to evaluate the efficacy of different systems of PPC.
Introduction
A recent report of the WHO coinciding with the 30th anniversary of Alma-Ata declaration has reinforced the concept of primary care as a key tool for high-quality healthcare services.1 2
In recent years, there has been an increasing awareness and concern about the wide variation between countries regarding the care of children and adolescents at the primary care level.3 Differences in the patterns of paediatric primary care (PPC) found in European countries in 1999 have been reported by Katz et al4 in a landmark article. In that study, three different healthcare delivery systems were identifi ed: paediatrician-based, general practitioner-based and combined services. It has been recognised that economic, geographical and historical factors contribute to these variations.
The outcomes of the different models in terms of health in the primary care setting are not easy to measure and have not been extensively studied. However, assessment of health and quality of care at the primary care level is essential in order to compare the different healthcare systems in Europe and has implications for future healthcare planning.5 6
Although it would seem reasonable to consider that primary care paediatricians are probably the best trained and experienced professionals to ensure the quality of care for ambulatory paediatric patients,7 countries with no or few paediatricians in primary care have satisfactory results in terms of conventional healthcare indicators, such as neonatal and infant mortalities, which are probably more related to income per capita4 than to healthcare systems.
Recently, some concerns have been raised in a number of countries regarding the capability of general practitioners (GPs) or family doctors (FDs) to continue acting as gatekeepers for paediatric patients. Where these systems prevail, there is a trend to call on primary care earlier in the evolution of a child’s illness and a higher demand on hospitals for emergency assessment when parents feel their children are ill.8 9
Inappropriate referral of patients by non-paediatricians is another area of concern and is a problem that has not been extensively investigated. In a Finnish study which examined the reasons for referral from the GP to hospitals, otitis media was the most common cause of referral in patients younger than 15 years of age.10 Moreover, the role of nurses in the different models has not been extensively studied. This aspect is particularly interesting because in some countries, a considerable work load is covered by these healthcare professionals, which in turn may contribute substantially to the effi ciency of the system.11
The aim of the present study was to present a general overview of the main characteristics of to whom, how and where PPC is delivered in the different European countries and the main problems each of the existing models is facing. This information will be useful to defi ne the current PPC profi le in Europe.
Methods
A questionnaire, which was partly based on the instrument used by Katz et al4 was developed by one of the authors (DvE) and approved by the coauthors of the study and the members of the Primary–Secondary Working Group (PSWG) of the European Academy of Paediatrics (EAP).
The study questionnaires with an accompanying letter explaining the purpose of the study were sent electronically by one of the authors (DvE) to each delegate of the 31 countries represented in the EAP. The delegates of all countries were active paediatricians working in PPC, secondary care or public health but well acquainted with the structure and functioning of paediatric care in the primary level. Completed questionnaires were collected from November 2007 to April 2008.
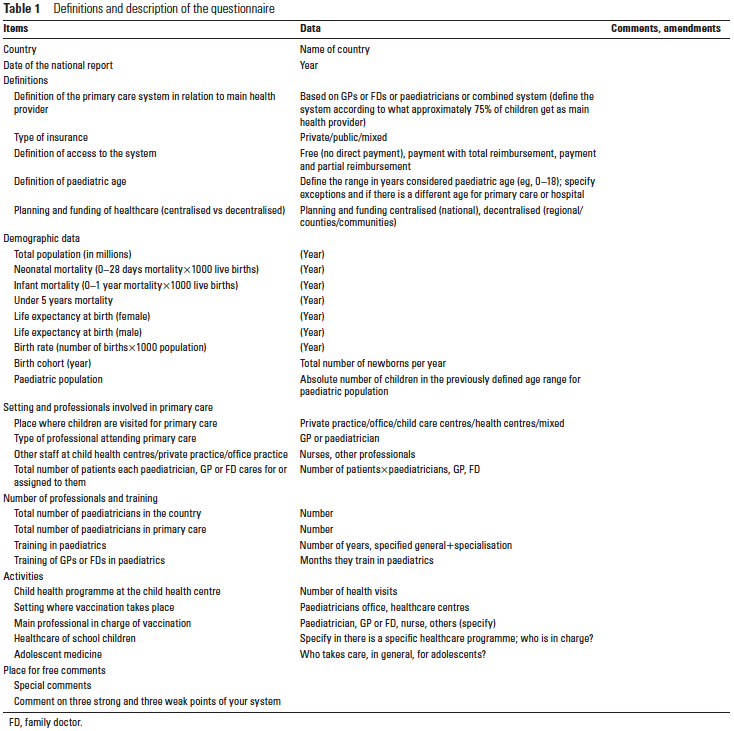
The questionnaire was divided into six sections: (A) defi nitions of the primary paediatric care system, (B) demographic data, (C) setting and professionals involved in primary care, (D) number of professionals and details of their training, (E) other activities and (F) a fi nal section for free comments on the strong and weak points of the primary care system of each country. Details of the questionnaire are shown in table 1. The classifi cation of the PPC systems was made according to the professionals (paediatrician or GP/FD) caring for more than 75% of the paediatric population in the public healthcare system of each participating country. In the combined (mixed) system, both paediatricians and GPs/FDs offer care in a varied proportion. All European countries included in this survey have public healthcare insurance systems at the primary care level which care for most of the paediatric patients. Access is totally free in most of them and reimbursed in the rest.
Population demographic data and health indicators were obtained from the Eurostat website at http://ec.europa.eu/ eurostat, from the Unicef website at http://www.childinfo.org or from national data. Some data referring to professional practice were estimates made by the representatives of each country.
Results
The results reported are from the responses received from 29 of the 31 countries that belong to the PSWG of the EAP and to whom the questionnaire was sent: 25 of 27 (92.6%) European Union countries, three from European Free Trade Association countries (Switzerland, Iceland and Norway) and one from an associate member country (Israel).
Demographic data
The total population from the 29 countries included in the study was 491 011 230 inhabitants, with a paediatric population of 90 795 307 and annual birth cohort of 5 153 295 infants. The proportion of the paediatric population with respect to the total population varied between 14.13% for Italy and 32.4% for Israel.
Definitions of the primary paediatric care system
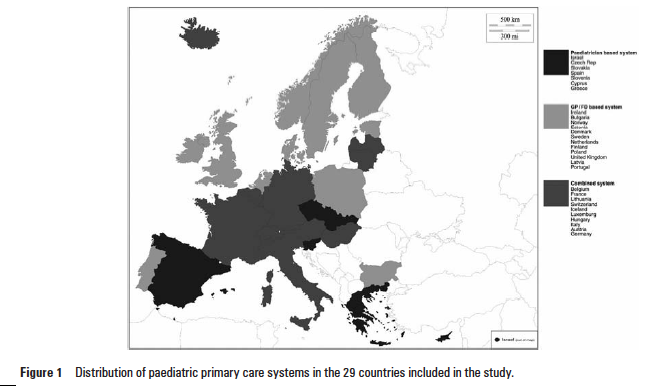
Seven (24.1%) had a paediatrician-based system for primary care of children, 12 of the 29 (41.4%) countries had a GP/FD system, and 10 (34.5%) had a combined system. Figure 1 shows the countries belonging to the different systems.
The type of insurance was public in 82.8% of the countries and mixed (private/public) in the remaining 17.2%. Access to the system was free with no direct payment in 75.9% of the countries and with payment and partial reimbursement in 24.1%. Planning and funding of healthcare were centralised in 24 countries (82.8%) and decentralised in five.
The definition of the paediatric age at the primary care leve varied across Europe. The majority (15 countries) defi ned the paediatric age up to 18 years of age, with the remaining 48% distributed from a low of 14 years (17%) to a maximum of 19 years in 10%. In several countries, the age is extended to adulthood for hospital admissions or for specialised care (eg, chronic conditions). Of the 11 countries with a paediatric age lower than 0–18, eight of them have an extended paediatric age to 18 years or higher in case of hospitalisation.
Clinical setting and professionals involved in primary care
With regard to the place where children are visited for primary care, these took place in private offi ces in nine countries, in child/healthcare centres in eight, and in both private offi ces and healthcare centres in 12.
For the variable of the number of patients each primary care professional (paediatrician or GP/FD) cares for, data were available only for 21 countries. The median number of patients each paediatrician or (GP/FD) has under their care was 1250 (range 650–2100).
Data for other staff present at the primary care level were missing for four countries. For the remaining 25 countries, nurses were present in the primary care setting in 16 countries (64%) and nurses and other professionals in nine countries. The number of nurses per paediatrician or GPs/FDs was 1 (median of 1; range 1–7).
Number of professionals and training
The total number of paediatricians working in the countries included in the study was 82 078, 40.4% of which (n=33 195) were working in the primary care setting.
The standard training recommended by the European Board of Paediatrics (Standing Committee of the EAP) is 5 years, composed of 3 years for the common trunk and 2 years each for specialised training in either primary, secondary or tertiary care.
The number of training years in paediatrics was 5 years or more for 20 of the 29 countries and less than 5 years in nine countries. The median time for training of a GP or a FD in paediatrics was 4 months (IQR 3–6), with some countries not having any compulsory paediatric training at all.
Activities
The mean number of health visits scheduled in the context of the child’s health programme throughout the years of care of each country was 14.7 (range 5–30). Vaccinations were administered at the paediatrician’s offi ce in eight countries, in the healthcare centre in nine and in multiple locations in 12. Professionals involved in vaccination included nurses in five countries (Sweden, Portugal, Israel, Finland, Norway), paediatricians in fi ve (Bulgaria, Czech Republic, Germany, Greece, Slovakia), GPs/FDs in fi ve (Poland, Ireland, Estonia, Denmark, Belgium) and a combination of professionals in 12 countries.
Data from 25 countries were available on whether or not some kind of specifi c healthcare programme for schoolchildren was present. Twenty-two countries had specifi c healthcare programmes, and three did not. Doctors and nurses were in charge of the programme in six countries, school health nurses in three, paediatricians in three and paediatricians and GPs/FDs in seven. Twenty-two countries furnished data regarding who is mainly responsible for adolescent medicine. Paediatricians were in charge of adolescent medicine in five and GPs/FDs in another fi ve, and a mixed care (GPs mainly and occasionally paediatricians) was the predominant system in 14 countries.
Discussion
Recently, the WHO released its World Health Report 2008 with the slogan ‘primary health care, now more than ever,’1 reinforcing once again the need for well-developed primary care as a key element for the quality of any healthcare system. The present study gives a general overview of PPC in Europe, with the aim of sharing information among countries with different primary care models. The controversy regarding which is the best system for children’s care at the primary care level is still ongoing due, in part, to the fact that accurate and reliable data concerning effi cacy of the various systems are insuffi cient at the present moment.
Regarding the type of PPC system, only seven countries (24%) still have a paediatrician-based system. Ten countries (35%) have a combined system, and 12 (41%) a system based on GPs/FDs. In comparison with the previous study of Katz et al,4 there is an increase in the GPs/FDs systems and a decrease in both the combined and the paediatrician-based systems (figure 2). However, these differences may be partly due to the use of different definitions for classifying countries to one or another group. In our study, defi nitions of the systems were based on the type of care provided by the public health insurance system which is the main provider for healthcare in the surveyed countries. For example, Portugal was assigned to the combined system by Katz et al4 and as a GP/FD system in our study, due to the fact that although there are private paediatricians working in primary care, the Portuguese public healthcare system includes GPs only as primary care doctors for children. Bulgaria changed, in 2001, from a paediatricianbased system to a GP-based system. The shortage of paediatricians to attend the demands of the primary care population in different countries with a paediatrician-based structure may anticipate changing over to a combined system in the near future if changes in the number of postgraduates willing to work in primary care and the organisation of the professional practice are not urgently considered.
Interestingly, there is a large variation in the defi nition of paediatric age used in the different countries at the primary care level. In more than half of the countries, paediatric age is defi ned as 0–18 years, but in 38% of the countries, paediatric age is up to 14, 15 or 16 years. In most countries, hospital admissions and follow-up by subspecialists, especially in case of chronic diseases, is extended up to 18 years. Harmonisation of the defi nition of paediatric age for all European countries would be desirable at the primary, secondary and tertiary care levels, as well as fi xing age limits for hospitalisation.
Rigby et al12 described a series of healthcare indicators for the European paediatric population in the context of the Child Health Indicators of Life and Development project. A total of 38 core indicators, which would be useful to measure the paediatric healthcare status were identifi ed. The use of these indicators could be helpful to assess more precisely differences between the various systems. Unfortunately, complex data are required for the calculation of most of these indicators, and the data are not available in the majority of countries.
Training in paediatrics received by GPs or FDs is clearly insufficient, with a median of only 4 months. In some countries, paediatric training for GPs or FDs is not compulsory or even non-existent. This is probably a major problem faced by those countries with no paediatricians at the primary care level. There are, at present, no clear data on how long GPs or FDs should train in paediatrics to be able to care with sound knowledge for paediatric patients. Training between 9 and 12 months is probably the minimum required to acquire a basic knowledge of the specifi c healthcare problems of the paediatric patients which are not covered in the training programmes of GPs or FDs.
The number of preventive child health examinations included in the different systems varied considerably from a few visits in some countries (fi ve in Luxemburg and eight in Denmark) to a large number in others (more than 20 in Slovakia, Latvia, Lithuania and Sweden). Prevention is important in maintaining good health in our children, but evidence for the best routine screening programme is lacking. Some countries, such as The Netherlands, have a system which includes preventive care doctors, and with this system, a high level of compliance of the programmes is achieved. In other countries, preventive health checks are conducted by nurses, paediatricians or GPs/FDs. A recent study highlights that utilisation of preventive child health examinations is lower among the more socially disadvantaged segments of the population.13
Heterogeneity of the systems and organisations of PPC in Europe should be regarded as an opportunity to compare and obtain information on their quality. However, more sensitive and specific healthcare indicators, which should be routinely and uniformly collected in all countries, are necessary.
Acknowledgements
The authors thank JL Bonal (Spain) and J Ruiz-Canela (Spain), for supporting the activities of DvE at the European Academy of Paediatrics (EAP); M Zach, P Hamilton, A Tenore and J Ramet, from the EAP; A Craft, for helpful criticisms and valuable comments; and M Pulido for editorial assistance. Contributors of the PSWG: I Azevedo (Portugal), S Barak (Israel), A Barillari (Belgium), A Biver (Luxembourg), F Bovet (Switzerland), A Chybicka (Poland), C de Beaufort (Luxembourg), S del Torso (Italy), AK Eigenmann (Switzerland), Ü Einberg (Estonia), E Ghenev (Bulgaria), A Hadjipanayis (Cyprus), P Hamilton (UK), H Hardarson (Iceland), E Jaeger-Roman (Germany), F Kadar (Hungary), G Kubatova (Czech Republic), I Lanka (Latvia), R Lounamaa (Finland), F Mimouni (Israel), A Nicholson (Ireland), K Prcuchova (Slovakia), A Prieler (Austria), F Rubel (France), O Rudzeviciene (Lithuania), W Sedlak (Austria), MS Zupancic (Slovenia), E Siebke (Norway), K Simovicova (Slovakia), F Skovby (Denmark), M Solomou (Cyprus), D Stefanidis (Greece), N Szitanyi (Czech Republic), D Van Esso (Spain), P Verloove Vanhorick (Netherlands) and B Wettergren (Sweden).
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
References
1. Primary health care—now more than ever. The World Health Report 2008. World Health Organization, 2008.
2. Rawaf S, De Maeseneer J, Starfi eld B. From Alma-Ata to Almaty: a new start for primary health care. Lancet 2008;372:1365–7.
3. Ercan O, Alikasifoglu M, Erginoz E, et al. Demography of adolescent health care delivery and training in Europe. Eur J Pediatr 2009;168:417–26.
4. Katz M, Rubino A, Collier J, et al. Demography of pediatric primary care in Europe: delivery of care and training. Pediatrics 2002;109:788–96.
5. del Torso S, Bussi R, DeWitt TG. Primary care pediatrics in Italy: eighteen years of clinical care, research, and teaching under a national health service system. Pediatrics 1997;99:E8.
6. Janda J. Paediatric care in the Czech Republic. Arch Dis Child 1995;72:271–3.
7. Cheng TL. Primary care pediatrics: 2004 and beyond. Pediatrics 2004;113:1802–9.
8. Peile E. The future of primary care paediatrics and child health. Arch Dis Child 2004;89:113–15.
9. Craft A. Out of hours care. Arch Dis Child 2004;89:112–13.
10. Vehviläinen AT, Kumpusalo EA, Takala JK. Reasons for referral from general practice in Finland. Scand J Prim Health Care 1997;15:43–7.
11. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002;324:819–23.
12. Rigby MJ, Köhler LI, Blair ME, et al. Child health indicators for Europe: a priority for a caring society. Eur J Public Health 2003;13:38–46.
13. Søndergaard G, Biering-Sørensen S, Michelsen SI, et al. Non-participation in preventive child health examinations at the general practitioner in Denmark: a register-based study. Scand J Prim Health Care 2008;26:5–11.
Click here to download the presentation



